- Systematic Review
- Open access
- Published:
Efficacy of CEUS-guided biopsy for thoracic and pulmonary lesions: a systematic review and meta-analysis
BMC Medical Imaging volume 25, Article number: 158 (2025)
Abstract
Background
This study compares the success rate, diagnostic accuracy, and safety of contrast-enhanced ultrasound (CEUS)-guided biopsy versus conventional ultrasound (US)-guided biopsy for thoracic and pulmonary lesions.
Methods
A systematic search of PubMed, EMBASE, Web of Science, and Cochrane Library was conducted. The primary outcomes included success rate and diagnostic accuracy, and the secondary outcome was the odds ratio of adverse effects. A random-effects meta-analysis pooled the data, with heterogeneity assessed by I² and publication bias evaluated using Egger’s test and funnel plot analysis. Sensitivity analysis was performed to confirm result robustness. Subgroup analysis and meta-regression were conducted to explore the sources of heterogeneity.
Results
Sixteen studies with 3,459 patients were included. CEUS-guided biopsy demonstrated higher success rate (99.18%, 95% CI: 98.00-99.90%) and diagnostic accuracy (95.96%, 95% CI: 94.84-96.96%) than US-guided biopsy (success rate: 97.26%, 95% CI: 95.45-98.68%; diagnostic accuracy: 85.87%, 95% CI: 82.05-89.31%). Complications were more frequent in the US-guided group, with an odds ratio of 1.65 (95% CI: 1.15–2.37). Heterogeneity was low, and publication bias was minimal, except for diagnostic accuracy in the US group. Sensitivity analysis confirmed result robustness.
Conclusion
Compared with conventional ultrasound, CEUS-guided biopsy demonstrates a comparable success rate, superior diagnostic accuracy, and a lower incidence of complications, underscoring its clinical value as a preferred approach for thoracic and pulmonary lesion assessment.
Systematic review registration
This study was registered with PROSPERO under the registration number CRD42024608627.
Clinical trial number
Not applicable.
Introduction
Thoracic and pulmonary lesions present complex diagnostic challenges, with percutaneous transthoracic needle biopsy playing a pivotal role for confirming malignancy and guiding treatment strategies [1, 2]. Compared to computed tomography (CT) guided biopsy, ultrasound (US) guided biopsy offers several advantages, including lower cost, portability for bedside procedures, absence of radiation exposure, time efficiency, and real-time visualization [3]. However, conventional US-guided biopsies are often limited by their inability to reliably distinguish necrotic from viable tissue, which can result in false-negative findings and delays in diagnosis and treatment [4, 5]. Furthermore, complications such as pneumothorax and bleeding can complicate the procedure and increase patient risk [5].
In recent years, contrast-enhanced ultrasound (CEUS) has garnered growing attention for its ability to improve biopsy outcomes by providing enhanced visualization of lesion vascularity and tissue perfusion [6, 7]. Unlike CT and magnetic resonance imaging (MRI) contrast agents, the microbubbles used in CEUS are small enough to pass through capillary beds but too large to enter the interstitial space. This enables CEUS to enhance vessels as small as 50 μm, far below the detection threshold of power Doppler ultrasound, where blood flow is often too slow to be distinguished from surrounding tissue motion [8]. This enhanced visualization allows for more precise targeting of viable tissue during biopsies by differentiating between perfused and necrotic areas [8,9,10].
Despite these potential advantages, the clinical superiority of CEUS over conventional US remains unclear, with some studies reporting conflicting results, particularly in smaller lesions or in cases with extensive necrosis [4, 11]. Furthermore, the limited sample sizes and non-randomized designs of many existing studies make it difficult to draw definitive conclusions about the true benefits of CEUS in guiding biopsies for thoracic and pulmonary lesions.
This meta-analysis seeks to address these knowledge gaps by systematically reviewing and synthesizing the available evidence on the efficacy of CEUS-guided biopsy. By comparing success rates, diagnostic accuracies, and complication rates between CEUS and US-guided biopsy, we aim to provide robust, evidence-based recommendations that can inform clinical practice. Additionally, we will explore the performance of CEUS in different lesion types, including lung, mediastinum, and pleura, to offer a comprehensive understanding of its efficacy across a range of clinical scenarios.
Methods
Literature search
The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and registered with PROSPERO under the registration number CRD42024608627.
Initially, we conducted an exhaustive search of PubMed, EMBASE, Web of Science, and the Cochrane Library databases from their inception up to March 5, 2025, restricting our search published in English. Search terms targeting titles and abstracts included ‘thoracic and pulmonary’, ‘ultrasound’, ‘contrast-enhanced ultrasound’, and ‘biopsy’ to identify relevant studies. Detailed search strategies, partially adapted from Jacobsen et al. [9], can be found in the supplementary materials (Table S1 and Table S2). Duplicate records were identified and removed using EndNote’s built-in deduplication function. Additionally, we examined the reference lists of the included studies and used the Web of Science citation index to identify additional relevant research. Furthermore, we contacted the authors of the included studies and consulted field experts to obtain any additional relevant data.
Study eligibility
The search yielded articles that were independently assessed for eligibility by reviewers Z.S. and X.Y. Full-text reviews were conducted to confirm study inclusion. Disagreements were settled by consensus with the involvement of a third reviewer, B.Z.
The inclusion criteria were as follows: (1) primary research; (2) participants were patients with undiagnosed thoracic disorders or diseases; (3) Any studies with primary focus on biopsy procedures guided with CEUS compared with conventional ultrasound guidance in thoracic disorders or diseases; (4) articles were published in English; (5) the full text was available.
The exclusion criteria were as follows: (1) abstracts, case reports, conference presentations, reviews, editorials, and expert opinions, animal studies; (2) studies with a sample size of less than 10; (3) studies with overlapping datasets; (4) Studies primarily accessing cardiac structures, esophageal structures, central vessels (e.g. aorta, etc.) or mammary structures; (5) ultrasound contrast agents not administered intravenously; (6) studies involving lesions with a previous biopsy attempt and unsatisfactory pathology results.
Data extraction
In accordance with protocol, reviewers Z.S. and X.Y. independently extracted data following full-text review. The primary outcome of interest was the comparison of overall success and diagnostic rates between the US group and the CEUS group. The secondary outcome focused on the pooled odds ratio (OR) of adverse effects in the CEUS group relative to the US group. Additional data collected included the anatomic location of lesions, lesion sizes, contrast agent doses, standard references, and other pertinent variables.
The quality of the included studies was assessed using the Cochrane Risk of Bias (RoB) Tool for randomized controlled trials (RCTs) [12] and the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) for non-randomized studies [13]. Briefly, we evaluated each RCT across seven domains, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. Non-randomized studies were evaluated across seven bias domains, including confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes, and selection of the reported results. The risk of bias for each domain was rated as low, high, or unclear.
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to assess the certainty of evidence for the outcomes of interest [14]. Two authors (ZS and JM) independently performed the GRADE assessment, with disagreements resolved through discussion. The GRADE system assigns ratings of high, moderate, low, or very low to the certainty of evidence based on factors including risk of bias, inconsistency, imprecision, indirectness, and publication bias. RCTs were initially rated as high-certainty evidence, while non-RCTs were rated as low-certainty evidence. Each outcome was assessed for potential downgrading or upgrading according to these factors.
Definition of key parameters
The success rate was defined as the proportion of patients in whom a technically successful biopsy was performed, meaning that an adequate tissue sample was obtained for histopathological examination.
Diagnostic accuracy was defined as the proportion of cases in which the determinate biopsy diagnosis was consistent with the final diagnosis, relative to the total number of cases. The final diagnosis was based on either surgical pathology or clinical comprehensive assessment. It is important to note that in most cases where malignancy was confirmed through biopsy pathology, further surgical confirmation was generally not performed. Instead, personalized treatment was initiated based on the definitive pathological diagnosis, making it impossible to accurately determine false positives. False negatives were defined as cases in which the biopsy pathology indicated benign findings or yielded inconclusive results, but the final diagnosis confirmed malignancy.
In addition, procedure-related complications were assessed, including pneumothorax, bleeding, chest pain, and hemoptysis.
Statistical analysis
The meta-analysis was conducted using STATA version 16.0 (Stata Corporation, College Station, TX, U.S.A.). A random-effects model was chosen to account for potential variability between studies due to differences in study design, population characteristics, and interventions. Pooled success rates, diagnostic accuracies, and ORs of adverse effects were calculated. Results of individual studies and syntheses were tabulated and visually displayed using forest plots, which presented pooled effect estimates and 95% confidence intervals for each outcome. Heterogeneity was assessed using the I² statistic [15], with heterogeneity classified as low (25–49%), moderate (50–74%), or high (75–99%). Subgroup analyses and meta-regression were performed to explore potential sources of heterogeneity. In addition to forest plots, publication bias was assessed using funnel plot and Egger’s test, and sensitivity analyses were conducted by excluding individual studies one at a time, with results displayed in sensitivity analysis plots to assess the robustness of the overall findings. A p value < 0.05 was considered statistically significant. Missing summary statistics were handled using appropriate methods, including statistical imputation or by contacting the study authors directly. Data conversions were performed as needed to standardize outcome measures across studies, ensuring compatibility for synthesis and analysis.
Results
Search selection and quality assessment
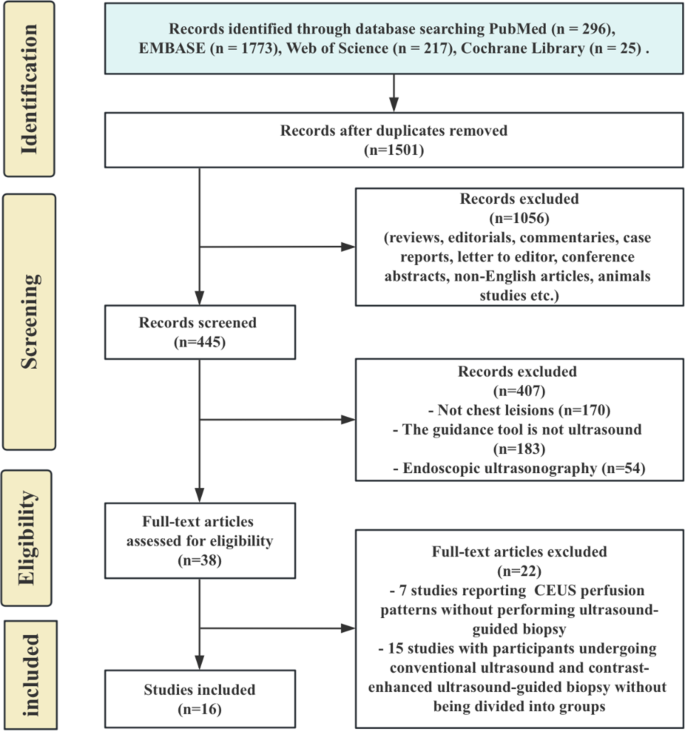
The study selection process is shown in Fig. 1. The initial search identified 1,501 unique records after duplicates were removed. After screening, 1056 records were excluded for reasons such as reviews, commentaries, case reports, or non-English articles. Of the remaining 445, 407 were excluded for reasons such as not addressing chest lesions, using non-ultrasound guidance, or employing endoscopic ultrasonography. After full-text review of 38 articles, 22 were excluded, leaving 16 studies for analysis.
In total, 16 studies with 3,459 patients were included [4, 5, 8, 11, 16,17,18,19,20,21,22,23,24,25,26,27]. Of these, 1,820 underwent US-guided biopsy and 1,639 underwent CEUS-guided biopsy. The characteristics and outcomes are summarized in Table 1. The studies included two randomized controlled trials, thirteen retrospective non-randomized studies, and one prospective non-randomized study. Nine studies focused on peripheral lung lesions, four on mediastinal lesions, two included both, and one addressed pleural lesion.
The quality assessment results indicate that the included RCTs generally had low to moderate risk of bias, primarily due to high risk in blinding of participants and personnel, while other domains were rated low or unclear (Table S3). For non-randomized studies, most were assessed as having a moderate risk of bias, with common issues in confounding, participant selection, and deviations from intended interventions (Table S4). These findings suggest that while the studies offer valuable insights, some methodological limitations should be considered when interpreting the results.
Pooled success rates of CEUS-guided and US-guided biopsy for thoracic and pulmonary lesions
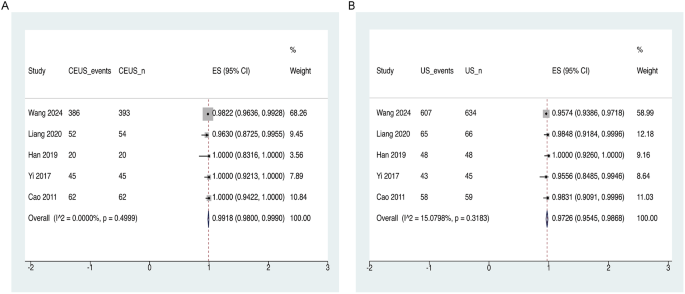
The meta-analysis demonstrated that the overall success rate of CEUS-guided biopsy was comparable to that of US-guided biopsy (Fig. 2). The pooled success rate for CEUS-guided biopsy was 99.18% (95% CI: 98.00-99.90%), with individual study rates ranging from 96.30 to 100%. (Fig. 2A). Heterogeneity among CEUS-guided studies was minimal (I² = 0.00%, p = 0.500). In contrast, the pooled success rate for US-guided biopsy was 97.26% (95% CI: 95.45-98.68%), with success rates ranging from 95.56 to 100% (Fig. 2B). US-guided studies also exhibited minimal heterogeneity (I² = 15.08%, p = 0.318).
Forest plots depicting the success rates of CEUS- and US- guided biopsies for thoracic and pulmonary lesions. (A) Overall success rate for CEUS-guided biopsy across all included studies, with pooled estimates and 95% CI. (B) Overall success rate for US-guided biopsy, with pooled estimates and 95% CI. Abbreviations: CEUS, contrast-enhanced ultrasound; CI, confidence interval; US, ultrasound
The funnel plots for both the CEUS-guided group (Fig. S1A) and the US-guided group (Fig. S1B) were symmetrical, indicating minimal publication bias. Furthermore, Egger’s test results for both groups yielded p-values greater than 0.1, further confirming the absence of significant publication bias (Table S5). The leave-one-out sensitivity analysis indicated that excluding any single study did not substantially affect the pooled estimates. However, the study by Wang 2024 exhibited a wider confidence interval, with its estimate falling outside the overall pooled confidence intervals, suggesting that this study may have had a considerable impact on the overall results (Fig. S1C and D).
Diagnostic accuracies of CEUS-guided and US-guided biopsy for thoracic and pulmonary lesions
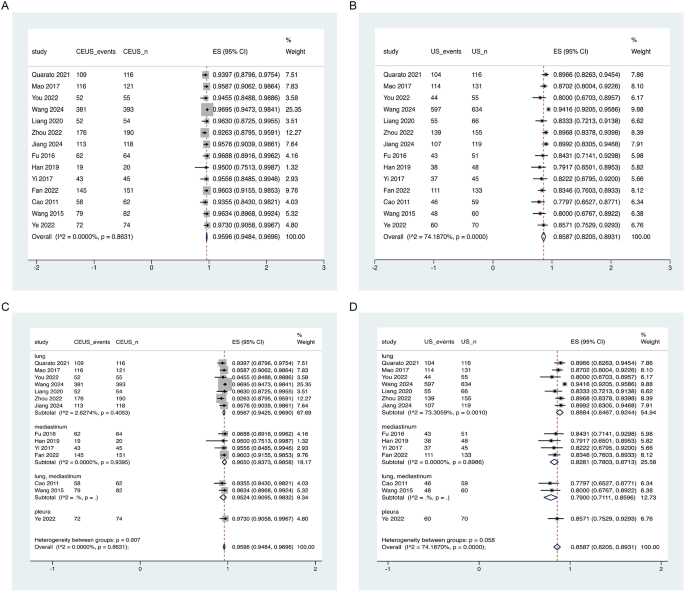
The meta-analysis revealed a higher overall diagnostic accuracy for CEUS-guided biopsy compared to US-guided biopsy (Fig. 3).
Forest plots of diagnostic accuracy for CEUS- and US-guided biopsies. (A) Overall diagnostic accuracy for CEUS-guided biopsy across included studies, with pooled estimates and 95% CI. (B) Overall diagnostic accuracy for US-guided biopsy, showing pooled estimates and 95% CI. (C) Subgroup analysis of diagnostic accuracy for CEUS-guided biopsy by lesion location. (D) Subgroup analysis for US-guided biopsy by lesion location. Heterogeneity statistics (I²) are provided at the bottom of each plot to indicate variability across studies. Abbreviations: CEUS, contrast-enhanced ultrasound; CI, confidence interval; US, ultrasound
The diagnostic accuracy of CEUS-guided biopsy was consistently high, with a pooled accuracy of 95.96% (95% CI: 94.84-96.96%). Individual study accuracy rates ranged from 92.63 to 97.30%, and heterogeneity was minimal (I² = 0.00%, p = 0.863) (Fig. 3A). Subgroup analysis based on lesion location showed an accuracy of 95.67% (95% CI: 94.25-96.90%) for lung lesions, 96.50% (95% CI: 93.73-98.58%) for mediastinal lesions, and 95.24% (95% CI: 90.95-98.32%) for studies involving both lung and mediastinal lesions (Fig. 3C). Heterogeneity across subgroups was minimal (I² = 2.63%, p = 0.405) and (I² = 0.00%, p = 0.940), indicating a high level of consistency.
In contrast, the pooled diagnostic accuracy for US-guided biopsy was lower at 85.87% (95% CI: 82.05-89.31%), with individual study rates ranging from 77.97 to 94.16% (Fig. 3B). moderate heterogeneity was observed (I² = 74.19%, p < 0.0001). Subgroup analysis showed that lung lesion studies had an accuracy rate of 88.84% (95% CI: 84.67-92.44%), mediastinal lesions had an accuracy of 82.81% (95% CI: 78.03-87.13%), and studies involving both lung and mediastinal lesions had an accuracy of 79.00% (95% CI: 71.11-85.96%) (Fig. 3D). Moderate heterogeneity was present in the lung lesion subgroup (I² = 73.31%, p = 0.001), while minimal heterogeneity was found in the mediastinal subgroup (I² = 0.00%, p = 0.899).
In a subset of studies [8, 11, 16, 22,23,24, 27], counts of false negatives were available. In the CEUS-guided group (1,006 participants), 29 false negatives were reported, while 74 were observed in the US-guided group (1,237 participants). These results did not significantly impact the overall diagnostic performance.
The funnel plot for the CEUS-guided group (Fig. S2A) appeared relatively symmetrical, indicating minimal publication bias. In contrast, the funnel plot for the US-guided group (Fig. S2B) showed asymmetry, suggesting the presence of publication bias, which was further confirmed by Egger’s test (p < 0.05) (Table S5). The leave-one-out sensitivity analysis demonstrated that excluding any single study did not substantially alter the pooled estimates. However, the study by Wang 2024 showed a lower 95% confidence interval that fell outside the overall pooled confidence interval, suggesting that this study may have had a notable influence on the pooled estimates (Fig. S2C and S2D).
The meta-regression analysis found no significant association between age, lesion size, or needle size and diagnostic accuracy in both the CEUS-guided and US-guided biopsy groups (all p > 0.05), suggesting that these factors did not contribute to the observed heterogeneity in diagnostic accuracy (Table S6).
Adverse effects: pooled ORs for CEUS-guided and US-guided biopsy for thoracic and pulmonary lesions
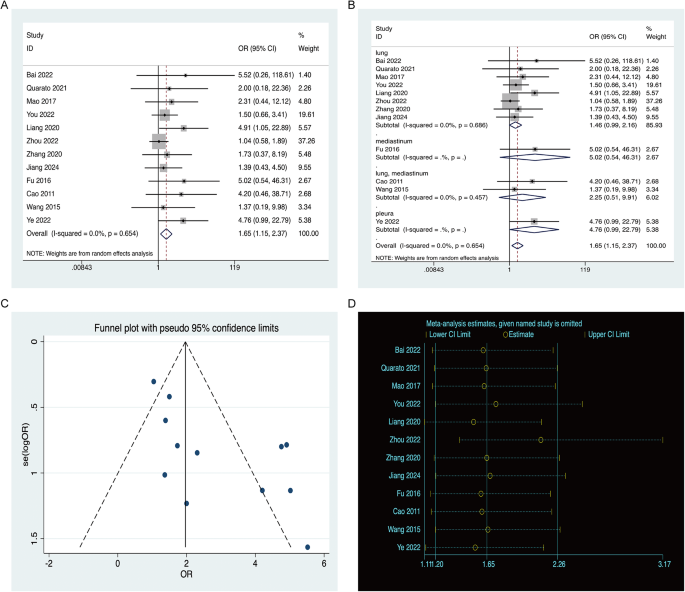
The pooled ORs for adverse effects associated with CEUS-guided and US-guided biopsy were analyzed, revealing an overall OR of 1.65 (95% CI: 1.15–2.37), suggesting a higher incidence of adverse effects in the US-guided biopsy group compared to the CEUS-guided group. Individual study ORs ranged from 1.37 to 5.52, with minimal heterogeneity across studies (I² = 0.00%, p = 0.654), indicating consistent results (Fig. 4A).
Forest plots for adverse effects associated with CEUS-guided and US-guided biopsies. (A) Pooled OR and 95% CI for adverse effects in studies comparing CEUS-guided and US-guided biopsy, where an OR greater than 1 indicates a higher incidence of adverse effects in the US-guided group relative to the CEUS-guided group. (B) Subgroup analysis by lesion location. (C) Funnel plot for publication bias assessment of adverse effects. (D) Leave-one-out sensitivity analysis. Abbreviations: CEUS, contrast-enhanced ultrasound; US, ultrasound; OR, odds ratio; CI, confidence interval
Subgroup analysis by lesion location further demonstrated that the increased odds of adverse effects in the US-guided biopsy group remained consistent across different lesion types. For lung lesions, the OR was 1.46 (95% CI: 0.99–2.16), while for mediastinal lesions, the OR was higher at 5.02 (95% CI: 0.54–46.31). Combined lung and mediastinal lesion studies reported an OR of 2.25 (95% CI: 0.51–9.91), and pleural lesions had an OR of 4.76 (95% CI: 0.99–22.79). Minimal heterogeneity was found in the lung subgroup (I² = 0.00%, p = 0.686), reinforcing the consistency of the results across different lesion locations (Fig. 4B).
The funnel plot revealed asymmetry (Fig. 4C), suggesting the presence of publication bias, which was further corroborated by Egger’s test (p < 0.05). The leave-one-out sensitivity analysis showed that excluding any single study did not substantially affect the pooled estimates. However, the study by Zhou 2022 exhibited a higher 95% confidence interval that extended beyond the overall pooled confidence interval, suggesting that this study may have had a notable influence on the pooled estimates (Fig. 4D).
GRADE assessment
The certainty of the evidence for meta-analytic outcomes was rated as low for success rate and very low for both diagnostic accuracy and adverse effects (Table S7). The main reasons for downgrading the evidence were risk of bias, inconsistency, and publication bias. Indirectness and imprecision were not downgraded, as this review adhered to strict eligibility criteria for population, intervention, comparator, and outcome.
Discussion
To our knowledge, this is the most comprehensive systematic review and meta-analysis to date assessing the success rate, diagnostic accuracy, and safety of CEUS-guided biopsy for thoracic and pulmonary lesions. In a 2022 systematic review by Jacobsen et al. [9], six studies comparing CEUS-guided and US-guided transthoracic needle biopsy of thoracic masses were analyzed, reporting a mean diagnostic accuracy of 95.4% for CEUS versus 80.8% for US. However, due to the limited number of studies, their review lacked a meta-analytic approach, relying instead on a descriptive synthesis. Additionally, four of the included studies focused exclusively on mediastinal lesions, with only one on peripheral lung lesions and one covering both, which may further restrict the generalizability of their conclusions. However, a meta-analysis by Zhang et al. published in 2023 specifically addressed thoracic ultrasound-guided pleural biopsy [28]. This study reported that CEUS-guided pleural biopsy achieved a diagnostic yield of 98.24%, which was significantly higher than the 78.97% yield from conventional US (p < 0.01). This emphasizes the potential of CEUS to enhance diagnostic accuracy for pleural lesions, further supporting its application in thoracic biopsies. Our study builds on these findings by providing a more robust meta-analytic assessment, reinforcing multifaceted advantages of CEUS for biopsy across diverse thoracic lesion types, beyond diagnostic accuracy. Our findings clearly demonstrate that, compared to conventional ultrasound, CEUS-guided biopsy offers a comparable success rate, superior diagnostic accuracy, and a lower incidence of complications. These results highlight the significant clinical advantages of CEUS over conventional ultrasound in guiding biopsies for thoracic and pulmonary lesions.
The enhanced visualization of lesion vascularity and tissue perfusion provided by CEUS is a critical factor [10, 20, 26]. By using microbubble contrast agents, CEUS dynamically highlights the blood flow within lesions, allowing for more precise targeting of viable tissue during biopsy and avoiding necrotic areas. This capability is particularly beneficial in thoracic and pulmonary lesions, where necrosis and vascular irregularities often complicate biopsy procedures [7, 29]. CEUS can visualize small vessels, down to 50 μm, further enhances its diagnostic accuracy, making it a valuable tool for improving biopsy success, especially in difficult-to-access lesions [8]. In contrast, conventional ultrasound, which relies on echogenicity to differentiate between tissue types, can lead to diagnostic errors when necrotic and viable tissues are not easily distinguishable.
Conventional ultrasound has several limitations that make it less suitable for accurately guiding biopsies in certain cases. It typically judges necrotic areas based on echogenicity, where low-echo or anechoic regions are assumed to be necrotic [4]. However, this approach can be imprecise, as ultrasound images may display varying echo levels, and biopsies of these areas often reveal necrotic rather than viable tissue. Moreover, conventional ultrasound can visualize larger blood vessels, but its ability to detect slow blood flow in smaller vessels is limited, particularly when patient cooperation or respiratory motion affects image quality [5]. This can lead to inaccurate biopsy site selection and an increased risk of complications. Additionally, conventional ultrasound may poorly identify necrotic and non-liquefied tissues, and color Doppler flow imaging is often affected by external factors such as the angle between the sound wave and blood vessels, resulting in reduced sensitivity and accuracy [17].
CEUS not only improves biopsy outcomes but also plays a critical role in the pre-procedural evaluation of lesions [30, 31]. It can be used to assess the qualitative characteristics of peripheral lung lesions, helping to differentiate between benign and malignant tumors based on their perfusion patterns [5, 6]. However, the presence of dual vascularization in the lung, originating from both the pulmonary and bronchial circulations—complicates the application of conventional CEUS protocols typically used in other organs. This dual supply creates challenges in accurately distinguishing perfusion patterns, which are crucial for assessing lesion viability and biopsy suitability. Studies have shown that malignant lesions often exhibit delayed enhancement due to their blood supply from bronchial arteries, while benign conditions such as pneumonia and atelectasis show early enhancement due to normal pulmonary perfusion [9]. Additionally, CEUS can determine whether a lesion is suitable for biopsy by evaluating its vascular characteristics and overall accessibility, thus preventing unnecessary invasive procedures in cases where a successful biopsy is unlikely [29].
Lesion size is another critical factor affecting the success of biopsy procedures [11, 27, 32, 33]. Larger lesions generally provide clearer ultrasound images, making localization easier and increasing the likelihood of successful tissue sampling and diagnostic accurately. However, larger lesions are also more prone to necrosis due to their rapid growth and the resulting mismatch between tumor vascularization and metabolic demands. CEUS plays a significant role in these cases by clearly identifying viable and necrotic areas, allowing for more precise targeting during biopsy and reducing the likelihood of sampling non-diagnostic necrotic tissue. Conversely, smaller lesions often present challenges due to their poorer image quality and susceptibility to respiratory motion, leading to lower success rate diagnostic accuracy and an increased need for multiple punctures. This, in turn, elevates the risk of complications such as pneumothorax and bleeding. Based on clinical experience and prior studies, it is recommended that CEUS be used prior to biopsy in lesions larger than 5 cm to ensure accurate tissue sampling and diagnostic accurately [8, 24, 25, 27]. It should be noted that hypoxic responses in tumors may lead to false-negative results, necessitating confirmation with CT scans.
It is important to note that CEUS-guided biopsy is most effective for lung lesions located strictly subpleural [31]. For lesions situated deeper within the lung parenchyma, the procedure becomes technically challenging due to air interposition, which obstructs clear visualization and renders the biopsy unfeasible.
Although the analysis revealed minimal heterogeneity in most of the pooled results, the diagnostic accuracy for the US-guided group exhibited moderate heterogeneity, suggesting variability in outcomes. Several factors may contribute to this heterogeneity, including patient demographics (such as age and comorbidities), lesion characteristics (such as size, location, vascularity, and pathology type), and procedural differences (such as operator experience and needle size). To assess potential confounders, meta-regression analyses were conducted on age, lesion size, and needle size. The results indicated that none of these factors significantly influenced diagnostic accuracy in either the CEUS-guided or US-guided biopsy groups. However, other potential confounders, such as operator experience, variations in biopsy techniques, and patient comorbidities, could still contribute to heterogeneity. Unfortunately, due to data limitations, further exploration of these factors was not possible. Future studies with more granular data and standardized protocols are needed to better address these sources of variability.
The study by Wang et al. (2024) [11] was identified as a potential influencer of the pooled estimates. Sensitivity analysis revealed a wider confidence interval for this study, with its estimate falling outside the overall pooled range, suggesting a notable impact on the results. Upon re-evaluating the study’s design and methodology, we found it to be a retrospective multicenter study with complete data, appropriate analytical methods, and a study population consistent with the other included studies. Furthermore, the key definitions used aligned with those in our analysis, enabling accurate data extraction. The observed phenomenon in the sensitivity analysis may be attributed to the significantly larger sample size of this study (393 participants in the CEUS group and 634 in the US group). After expert discussion, we decided to retain this study in the pooled analysis of success rate and diagnostic accuracy, as its inclusion did not undermine the overall robustness of the results.
Several limitations should be considered when interpreting the findings of this study. First, the majority of the included studies were non-randomized, which introduces the potential for selection bias and unaccounted confounding factors. Additionally, the relatively small sample sizes in certain subgroups, particularly for pleural lesions, may have limited the statistical power of subgroup analyses. Another limitation stems from the geographic concentration of the studies, with a significant proportion conducted in China, which may restrict the generalizability of our findings to other regions. Moreover, the inclusion of only English-language studies could have introduced language bias. Although publication bias analyses, including funnel plots and Egger’s test, suggested minimal bias, the possibility that unpublished studies with negative results may affect the overall conclusions cannot be excluded. Furthermore, while the leave-one-out sensitivity analysis confirmed the robustness of the pooled estimates, several studies exhibited 95% confidence intervals that extended beyond the overall pooled limits, suggesting the presence of unexplained heterogeneity. Potential sources of this heterogeneity, such as variations in operator experience, biopsy techniques, and patient comorbidities, were not fully explored due to limitations in the available data. These factors should be addressed in future research with more granular data and standardized methodologies.
Looking forward, large-scale, multicenter randomized controlled trials are essential to further validate the success rate, diagnostic accuracy, and safety of CEUS-guided biopsy. To provide more conclusive evidence of CEUS’s superiority over conventional ultrasound, especially in complex clinical situations involving necrotic or difficult-to-access lesions, additional trials are warranted. Furthermore, future studies should prioritize the adoption of standardized reporting criteria for patient comorbidities and the underlying causes of biopsy failure. This will help better understand their impact on outcomes and improve the consistency and comparability of results across studies. The integration of CEUS with advanced imaging techniques, such as elastography and microvascular imaging, shows significant promise in enhancing diagnostic precision, particularly in scenarios where conventional methods encounter limitations [34]. Continued advancements in CEUS technology and the optimization of biopsy protocols will be crucial for maximizing the clinical potential of this technique. Moreover, further research is necessary to explore the pre-biopsy application of CEUS as a tool for evaluating lesion viability and determining biopsy suitability, ultimately helping to reduce unnecessary invasive procedures.
Conclusions
This meta-analysis demonstrates that CEUS-guided biopsy achieves comparable success rates, superior diagnostic accuracy, and fewer complications compared to US-guided biopsy for thoracic and pulmonary lesions. The enhanced visualization offered by CEUS contributes to improved biopsy outcomes and helps minimize unnecessary procedures. While large, multicenter randomized trials are needed for further validation, the current evidence supports CEUS as a preferred technique for guiding biopsies, particularly in complex and challenging clinical cases.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CEUS:
-
Contrast-enhanced Ultrasound
- US:
-
Ultrasound
- CT:
-
Computed Tomography
- MRI:
-
Magnetic Resonance Imaging
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- RCT:
-
Randomized Controlled Trial
- RoB:
-
Cochrane Risk of Bias
- ROBINS-I:
-
Risk Of Bias In Non-randomized Studies of Interventions
References
Maxwell AWP, Abtin F, Fintelmann FJ, Baird GL, Suh RD, Sofocleous CT, et al. Transthoracic needle biopsy is a safe and effective diagnostic procedure. J Am Coll Radiol. 2024;21(4):545–6.
Sakai H, Takeda M. Percutaneous transthoracic needle biopsy of the lung in the era of precision medicine. J Thorac Dis. 2019;11(Suppl 9):S1213–5.
Ko JP, Shepard JO, Drucker EA, Aquino SL, Sharma A, Sabloff B, et al. Factors influencing pneumothorax rate at lung biopsy: are dwell time and angle of pleural puncture contributing factors? Radiology. 2001;218(2):491–6.
You QQ, Peng SY, Zhou ZY, Tan XL, Miao XS. Comparison of the value of conventional ultrasound and Contrast-Enhanced ultrasound-Guided puncture biopsy in different sizes of peripheral pulmonary lesions. Contrast Media Mol Imaging. 2022;2022:6425145.
Bai Z, Liu T, Liu W, Li Z, Zheng H, Li X. Application value of contrast-enhanced ultrasound in the diagnosis of peripheral pulmonary focal lesions. Med (Baltim). 2022;101(29):e29605.
Bi K, Zhou RR, Zhang Y, Shen MJ, Chen HW, Cong Y, et al. US contrast agent arrival time difference ratio for benign versus malignant subpleural pulmonary lesions. Radiology. 2021;301(1):200–10.
Safai Zadeh E, Görg C, Prosch H, Jenssen C, Blaivas M, Laursen CB, et al. WFUMB technological review: how to perform Contrast-Enhanced ultrasound of the lung. Ultrasound Med Biol. 2022;48(4):598–616.
Quarato CMI, Cipriani C, Dimitri L, Lacedonia D, Graziano P, Copetti M, et al. Assessing value of contrast-enhanced ultrasound vs. conventional transthoracic ultrasound in improving diagnostic yield of percutaneous needle biopsy of peripheral lung lesions. Eur Rev Med Pharmacol Sci. 2021;25(18):5781–9.
Jacobsen N, Pietersen PI, Nolsoe C, Konge L, Graumann O, Laursen CB. Clinical applications of Contrast-Enhanced thoracic ultrasound (CETUS) compared to standard reference tests: A systematic review. Ultraschall Med. 2022;43(1):72–81.
Sidhu PS, Cantisani V, Dietrich CF, Gilja OH, Saftoiu A, Bartels E, et al. The EFSUMB guidelines and recommendations for the clinical practice of Contrast-Enhanced ultrasound (CEUS) in Non-Hepatic applications: update 2017 (Long Version). Ultraschall Med. 2018;39(2):e2–44.
Wang XY, Yuan ZF, Gan KH, Zhong Y, Huang JX, Huang WJ, et al. Contrast-enhanced imaging in peripheral pulmonary lesions: the role in US-guided biopsies. Radiol Cardiothorac Imaging. 2024;6(3):e230234.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Mao F, Dong Y, Ji Z, Jin Y, Wang W. Comparison of contrast-enhanced ultrasound and conventional ultrasound for guiding peripheral pulmonary biopsies. Int J Clin Exp Med. 2017;10(2):3677.
Liang J, Wang D, Li H, Zhao S, Chen M, Li H, et al. Contrast-enhanced ultrasound for needle biopsy of thoracic lesions. Oncol Lett. 2020;20(4):75.
Zhou D, Zhang Y, Chen W, Jiang J, Chen Y, Zhou X, et al. Enhanced ultrasound-guided versus non-enhanced ultrasound-guided percutaneous needle biopsy in tissue cellularity of lung malignancies: a propensity score matched study. Quant Imaging Med Surg. 2022;12(11):5056–67.
Zhang H, Guang Y, He W, Cheng L, Yu T, Tang Y, et al. Ultrasound-guided percutaneous needle biopsy skill for peripheral lung lesions and complications prevention. J Thorac Dis. 2020;12(7):3697–705.
Fu J, Yang W, Wang S, Bai J, Wu H, Wang H, et al. Clinical value of contrast-enhanced ultrasound in improving diagnostic accuracy rate of transthoracic biopsy of anterior-medial mediastinal lesions. Chin J Cancer Res. 2016;28(6):617–25.
Han J, Feng XL, Xu TY, Feng WQ, Liu MJ, Wang B, et al. Clinical value of contrast-enhanced ultrasound in transthoracic biopsy of malignant anterior mediastinal masses. J Thorac Dis. 2019;11(12):5290–9.
Yi D, Feng M, Wen Ping W, Zheng Biao J, Fan PL. Contrast-enhanced US-guided percutaneous biopsy of anterior mediastinal lesions. Diagn Interv Radiol. 2017;23(1):43–8.
Fan P, Cao J, Jin Y, Han H, Wang W, Xu H, et al. Efficacy of contrast-enhanced ultrasound-guided percutaneous core needle biopsy in anterior mediastinal masses. J Interv Med. 2022;5(3):159–65.
Cao BS, Wu JH, Li XL, Deng J, Liao GQ. Sonographically guided transthoracic biopsy of peripheral lung and mediastinal lesions: role of contrast-enhanced sonography. J Ultrasound Med. 2011;30(11):1479–90.
Wang S, Yang W, Zhang H, Xu Q, Yan K. The role of Contrast-Enhanced ultrasound in selection indication and improveing diagnosis for transthoracic biopsy in peripheral pulmonary and mediastinal lesions. Biomed Res Int. 2015;2015:231782.
Ye F, Yang Y, Liu J. Comparison of High-Frequency Contrast-Enhanced ultrasound with conventional High-Frequency ultrasound in guiding pleural lesion biopsy. Ultrasound Med Biol. 2022;48(8):1420–8.
Jiang X, Chen J, Gu FF, Li ZR, Song YS, Long JJ, et al. Evaluating the efficacy of percutaneous puncture biopsy guided by contrast-enhanced ultrasound for peripheral pulmonary lesions. World J Clin Cases. 2024;12(19):3791–9.
Zhang Q, Deng MM, Li XL, Lu Y, Hou G. Thoracic ultrasound-guided real-time pleural biopsy in the diagnosis of pleural diseases: a systematic review and meta-analysis. Expert Rev Respir Med. 2023;17(9):805–13.
Yusuf GT, Fang C, Tran S, Rao D, Bartlett-Pestell S, Stefanidis K, et al. A pictorial review of the utility of CEUS in thoracic biopsies. Insights Imaging. 2021;12(1):9.
Hong-Xia Z, Wen H, Ling-Gang C, Wen-Jia C, Shuo L, Li-Juan D, et al. A new method for discriminating between bronchial and pulmonary arterial phases using Contrast-Enhanced ultrasound. Ultrasound Med Biol. 2016;42(7):1441–9.
Jiménez-Serrano S, Páez-Carpio A, Doménech-Ximenos B, Cornellas L, Sánchez M, Revzin MV, et al. Conventional and Contrast-enhanced US of the lung: from performance to diagnosis. Radiographics. 2024;44(7):e230171.
Liao WY, Chen MZ, Chang YL, Wu HD, Yu CJ, Kuo PH, et al. US-guided transthoracic cutting biopsy for peripheral thoracic lesions less than 3 cm in diameter. Radiology. 2000;217(3):685–91.
Guo YQ, Liao XH, Li ZX, Chen YY, Wang SD, Wang JH, et al. Ultrasound-Guided percutaneous needle biopsy for peripheral pulmonary lesions: diagnostic accuracy and influencing factors. Ultrasound Med Biol. 2018;44(5):1003–11.
Kuo YW, Chen YL, Wu HD, Chien YC, Huang CK, Wang HC. Application of transthoracic shear-wave ultrasound elastography in lung lesions. Eur Respir J. 2021;57(3).
Acknowledgements
Not applicable.
Funding
This study was funded by National High Level Hospital Clinical Research Funding (2022-NHLHCRF-LX-01-0205).
Author information
Authors and Affiliations
Contributions
B. Z. conceptualized the study design and led the protocol development. Z.S. and X.Y. conducted the systematic literature search, screened articles for eligibility, and performed data extraction. J.M. and T.Z. conducted the statistical analysis and data interpretation. Z.S. drafted the initial manuscript. All authors critically reviewed the manuscript, provided intellectual content, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, Z., Yu, X., Ma, J. et al. Efficacy of CEUS-guided biopsy for thoracic and pulmonary lesions: a systematic review and meta-analysis. BMC Med Imaging 25, 158 (2025). https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12880-025-01700-6
Received:
Accepted:
Published:
DOI: https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12880-025-01700-6